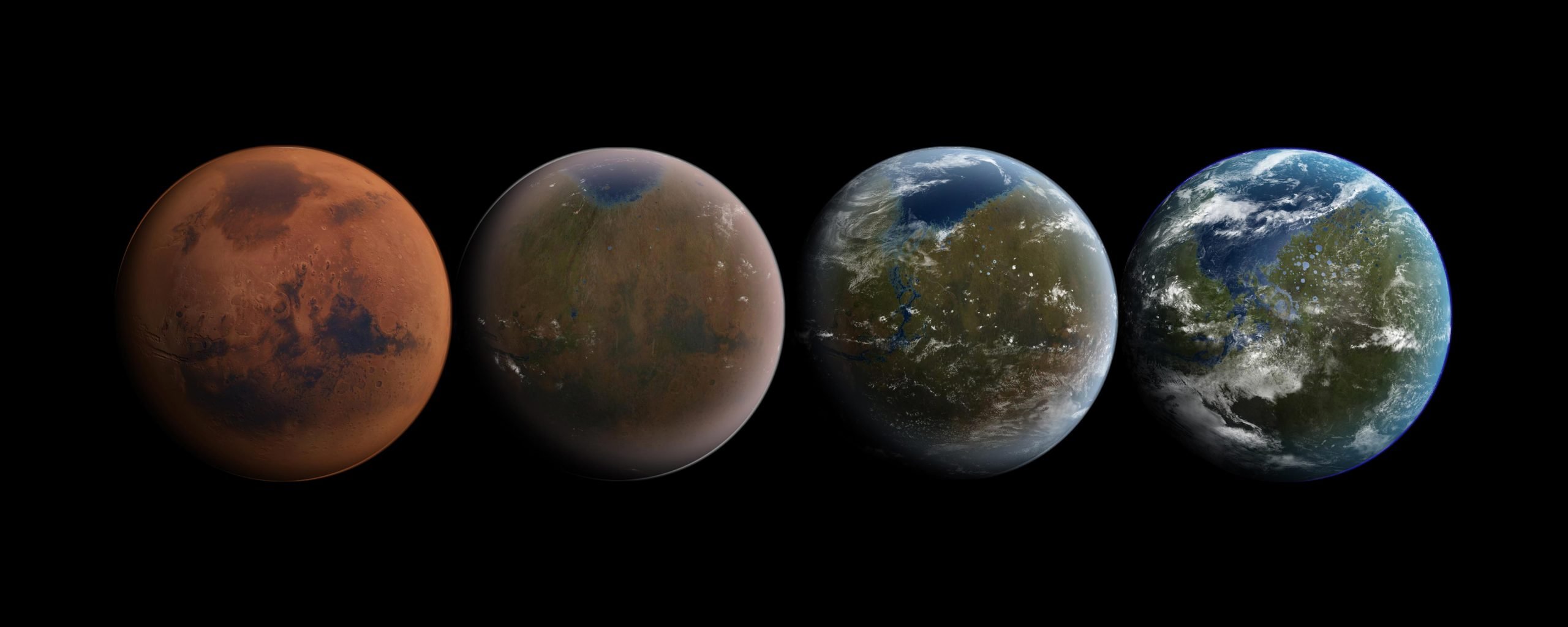
- Zopiclone is meant to be taken for two to four weeks as a short-term measure
- Have YOU suffered after taking zopiclone? Email [email protected]
Patients who were prescribed addictive ‘short-term’ sleeping pills by their GPs for years before being cut off suddenly with no support after an NHS rule change have revealed their crippling withdrawal symptoms.
Zopiclone, which was most common sleeping pill issued by GPs last year, is meant to be prescribed for two to four weeks as a temporary treatment due to the high risk of addiction and withdrawal being potentially fatal.
But users told MailOnline they have been given the drug for up to 10 years by their GP with no questions asked.
Thousands were then cut off suddenly when the NHS decided to crack down on potentially addictive medication, with no withdrawal plan or alternative in place.
They were left suffering panic attacks, muscle spasms, hallucinations and rebound insomnia – with no where to turn for help.
It follows the revelation that pregabalin, which is used by doctors to treat anxiety, epilepsy and nerve pain, is linked to thousands of deaths and has life-ruining side effects for those who use it.
Have YOU suffered after taking zopiclone? Email [email protected]
In total, NHS data shows GPs wrote 8million prescriptions for sleeping tablets last year at a cost of £89million to the health service.
In 2020, Public Health England found that some prescribed medicines like zopiclone were being given out inappropriately and for longer than recommended.
So the NHS introduced a new framework to tackle this, meaning GPs and clinical pharmacists have to provide patients with a personalised review and decide whether they should move away from using potentially addictive drugs.
And it succeeded – opioid prescriptions fell by 450,000 in just under four years.
The number of times zopiclone was put on a prescription in 2023 was 167,388 less than in 2021.
It appeared on prescription forms 368,442 times last year, according to NHS data.
But long-time users of the sleeping pill say they were cut off with ‘no warning’ and are suffering debilitating withdrawal symptoms.
Michele Clarke, 60, used zopiclone for 10 years. It was prescribed to combat the effects of Sertaline, an anti depressant which causes insomnia – and she said it ‘ruined my life’.
Her GP suddenly stopped her repeat prescription without any warning in May 2023 and she was told to take over-the-counter hay fever tablets instead.
She told MailOnline that she now suffers from stomach cramps and muscle spasms as she is still going through withdrawal. ‘Insomnia rules my life’, she said, adding that she was left near-suicidal over the symptoms.
After phoning 111 and getting paramedic call outs, she is now on a lower dosage of 3.5mg, taking four pills a fortnight to try wean herself off the drug.
But she admitted that it ‘doesn’t touch the sides after years of 7.5mg’ – and she won’t be able to get any more from April 1st.
Michele, who is Bipolar, also takes Diazapam for ‘manic episodes’ but also won’t be able to access it from April.
She’s been told to use the NHS website instead of getting a prescription from her GP, but there’s no option for either drug.
‘I have no where to get help,’ she said.
‘Millions who were prescribed powerful drugs like zopiclone, are suffering life damaging withdrawal symptoms and no plan by professionals to help them. An e-consult form is answered, but no help forthcoming.’
Describing her ordeal, she told MailOnline: ‘It has been the most terrible thing. I was calling centres which help people with addiction – and in a way it is addiction.
‘They offered me zopiclone as a means of sleeping but also of keeping me calm and for mood control. But then they decided last May, without any warning, to stop giving it to me.
‘They gave me 14 tablets and told me to make them last. They told me to buy over-the-counter hay fever tablets – I had no withdrawal plan. The advice was so poor.
‘I suffer from muscle cramps, shaking, vomiting, crying all the time. The anxiety is terrible, the nightmares I get are horrific.
‘When you go through withdrawal, you don’t think of anything else – your whole body is craving it. Your body is in so much pain.
‘I complained and complained and when my doctor finally saw me I asked “why didn’t you warn me?” I feel very let down. The government have done nothing.
‘It has had a huge impact on my life. I would wander around at 3am because I couldn’t sleep, and my neighbours were very concerned.
‘I didn’t realise how little my life was worth, how little my health was worth. I had black rings around my eyes and they were bloodshot. It is hell. It is just awful. I feel like I’m completely worthless. I can’t even play tennis anymore, I can’t do anything.’
Lara Ferguson, who is 25, took the highest dose of zopivlone – 7.5mg – for four years.
She became addicted but the sleeping pill stopped working because her body became so used to it.
Without any warning, her GP stopped her repeat prescription. She couldn’t sleep for days on end and was left feeling ‘scared and unstable’.
She was able to get it back, but her cries for help in reducing her dependency went unanswered until now.
This week she was moved to zolpidem and ‘finally can have a good night sleep’.
She said: ‘I first started zopiclone whilst on a psychiatric ward in London. I had been experiencing insomnia, which led me to self harming as I became extremely distressed.
‘When I was admitted I still couldn’t sleep and was staying up until 3-4am. I was told that I could be given zopiclone for seven days to help me get out of this acute period.’
Under current medical guidelines, GPs can prescribe a short course of sleeping pills for up to seven days.
The 25-year-old added: ‘My zopiclone was continued to be prescribed in the community long past these seven days. I soon developed a dependency and when I tried to stop it myself I couldn’t sleep at all, and experienced the highest levels of anxiety at night.
‘I was constantly on edge and felt hyper aware of everything. It was truly awful. So I continued to take the zopiclone as it seemed the only way forward.
‘The length of time I had been on it was never questioned by psychiatrists.
‘After being discharged from a unit two-and-a-half years ago my medication was controlled by my GP, who would only prescribe three doses per week.
‘By this point I was so dependent on the drug that I had to ring the GP practice on multiple occasions to beg them to give me a nightly dose.
‘Around four months ago I noticed that I started to experience insomnia again. I asked for a medication review but they said that I was on the right meds and doses, despite it now being almost four years on zopiclone.
‘Five weeks ago I was admitted to the general hospital for my anorexia. I was barely sleeping at all and experiencing rather traumatic nightmares. I explained to the medical staff here my situation, and they were horrified by how long I had been on zopiclone.
‘Two weeks ago I got a new psychiatrist who listened to my concerns and agreed to change my sleeping tablet to zolpidem.
‘Since then I have been able to get to sleep within an hour of taking it, which was unheard of before. I am getting far less nightmares and am only waking up once in the night, but can get straight back to sleep.
‘I am horrified that it took so long for people to recognise the length of time I’d been on the drug at the maximum dose.
‘Whilst I am pleased it has now been changed I’m worried that I am now reliant on sleeping medication.
‘I believe that patients should be given more information about the risks of dependency. By doing so people won’t experience the horrific withdrawal symptoms when the drug is no longer made available.’
Former model Claire Langdon, who is now 88, took zopiclone for ‘at least’ four years on a repeat prescription, which her daughter said turned her into a ‘zombie’.
Her daughter Annabel Christie told MailOnline: ‘I was shocked, because it was as if I had lost my mother.
‘She was showing symptoms of early dementia – she had lots of confusion, feeling very unwell. She would take them every morning when she woke up from taking them the night before – she wasn’t told otherwise.
‘She would be confused and a bit like a zombie. I did some research and told her “this pill doesn’t look good”.
‘I looked into it and I was horrified she was on a repeat prescription. The doctor said she would have to be weaned off it over the course of three to four months. She was feeling very low and had a lot of anxiety. I’m sure it was connected.
‘She was having delusions and was hallucinating. She had turned into a different person. I lost my mother for a while. When she came off them things improved.
‘It was horrendous, but she came through it. She’s now reluctant to take any sleeping pills at all after that.
‘They are really dangerous pills. I don’t think someone should be on them for longer than two weeks. It’s absolutely bonkers.’
When asked about what she thinks should be done to stop this from happening to others, she said: ‘They have to be more honest about the effects and how difficult and horrendous it is to come off them.
‘It was frightening to watch it happening. She got very anxious and her mood was very low. It was scary – we thought she was showing signs of dementia. But she doesn’t have it.
‘She had extreme tiredness, she was delusional and had extreme weakness. When she was taking it, her sleep pattern wasn’t much improved – it didn’t really work.’
Lee Hawker-Lecesne MBPsS, Clinical Director at luxury rehab centre The Cabin, said: ‘Prolonged use of zolpidem or zopiclone can lead to physical dependence, where the body adapts to the presence of the drug, and abrupt discontinuation can result in withdrawal symptoms.
‘Over time, individuals may develop tolerance, requiring higher doses to achieve the same sedative effects, which can increase the risk of dependence.
‘Withdrawal symptoms from zopiclone can include rebound insomnia – Individuals may experience a worsening of insomnia, which is often more severe than the original sleep difficulties.
‘Withdrawal can lead to increased levels of anxiety and irritability. In rare cases, withdrawal may lead to confusion and hallucinations.’
It follows the revelation that pregabalin, which is used by doctors to treat anxiety, has been linked to thousands of deaths.
Users told MailOnline how their lives were ‘destroyed’ by the drug – leaving them hallucinating ‘dead people’ and cats sitting on their laps just 30 minutes after taking the first dose.
It has been linked to nearly 3,400 deaths in Britain in the last five years alone, with the drug involved in 779 fatalities in 2022 – up from just nine a decade earlier in 2012, The Times reported.
Recent figures show it has the fastest rising death toll of any drug in the UK, and it is only behind opiates (such as heroin and morphine), cocaine and benzodiazepines (such as Valium and Xanax) in the number of fatalities it is linked to.
When MailOnline contacted the NHS, a spokesperson said: ‘There is strong evidence that long-term use of these drugs is dangerous for patients, and they should be supported to stop taking them when the benefits no longer outweigh the risks.
‘NHS guidance is clear that where this might be the case, patients should be involved in the decision and offered support, such as group counselling and peer support.’
A spokesperson for Sanofi, which manufactures the drug, told MailOnline: ‘Sanofi cannot comment on the use of zopiclone outside of its marketing authorisation and strongly recommend that any patient who is concerned about or is experiencing any side effects of a medicine contact their Healthcare Professional. ‘
Have YOU suffered after taking zopiclone? Email [email protected]

Sarah Carter is a health and wellness expert residing in the UK. With a background in healthcare, she offers evidence-based advice on fitness, nutrition, and mental well-being, promoting healthier living for readers.