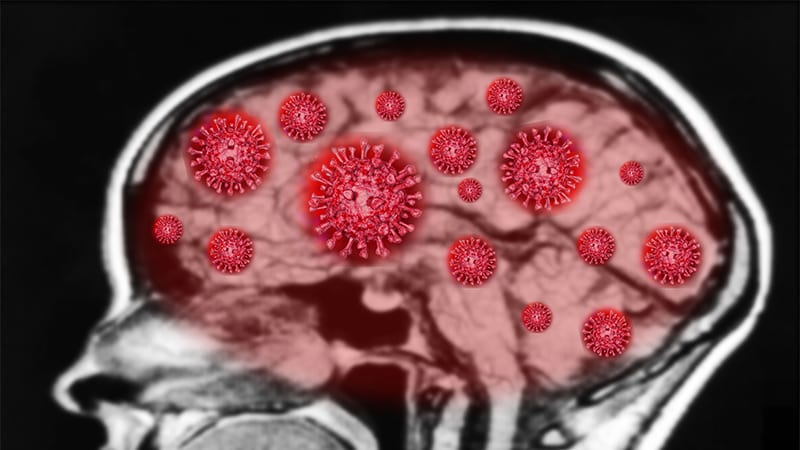
Brain fog is one of the most common, persistent complaints in patients with long COVID. It affects as many as 46% of patients who also deal with other cognitive concerns like memory loss and difficulty concentrating.
Now, researchers believe they know why. A new study has found that these symptoms may be the result of a viral-borne brain injury that may cause cognitive and mental health issues that persist for years.
Researchers found that 351 patients hospitalized with severe COVID-19 had evidence of a long-term brain injury a year after contracting the SARS-CoV-2 virus. The findings were based on a series of cognitive tests, self-reported symptoms, brain scans, and biomarkers.
Brain Deficits Equal to 20 Years of Brain Aging
As part of the preprint study, participants took a cognition test with their scores age-matched to those who had not suffered a serious bout of COVID-19. Then a blood sample was taken to look for specific biomarkers, showing that elevated levels of certain biomarkers were consistent with a brain injury. Using brain scans, researchers also found that certain regions of the brain associated with attention were reduced in volume.
Patients who participated in the study were “less accurate and slower” in their cognition, and suffered from at least one mental health condition, such as depression, anxiety, or posttraumatic stress disorder, according to researchers.
The brain deficits found in COVID-19 patients were equivalent to 20 years of brain aging and provided proof of what doctors have feared: that this virus can damage the brain and result in ongoing mental health issues.
“We found global deficits across cognition,” said lead study author Benedict Michael, PhD, director of the Infection Neuroscience Lab at the University of Liverpool in Liverpool, England. “The cognitive and memory problems that patients complained of were associated with neuroanatomical changes to the brain.”
Proof That Symptoms Aren’t ‘Figment’ of Patients’ Imaginations
Cognitive deficits were common among all patients, but the researchers said they don’t yet know whether the brain damage causes permanent cognitive decline. But the research provides patients who have been overlooked by some clinicians with proof that their conditions aren’t a figment of their imaginations, said Karla L. Thompson, PhD, lead neuropsychologist at the University of North Carolina School of Medicine’s COVID Recovery Clinic.
“Even though we’re several years into this pandemic, there are still a lot of providers who don’t believe that their patients are experiencing these residual symptoms,” said Thompson, “That’s why the use of biomarkers is important, because it provides an objective indication that the brain has been compromised in some way.”
Some patients with long COVID have said that getting their doctors to believe they have a physical ailment has been a persistent problem throughout the pandemic and especially as it relates to the sometimes-vague collection of symptoms associated with brain fog. One study found that as many as 79% of study respondents reported negative interactions with their healthcare providers when they sought treatment for their long-COVID symptoms.
How Do COVID-Related Brain Injuries Happen?
Researchers are unsure what’s causing these brain injuries, though they have identified some clues. Previous research has suggested that such injuries might be the result of a lack of oxygen to the brain, especially in patients who were hospitalized, like those in this study, and were put on ventilators.
Brain scans have previously shown atrophy to the brain’s gray matter in COVID-19 patients, likely caused by inflammation from a heightened immune response rather than the virus itself. This inflammatory response seems to affect the central nervous system. As part of the new study, researchers found some neuroprotective effects of using steroids during hospitalization to reduce brain inflammation.
The results suggest that clinicians should overcome their skepticism and consider the possibility that their patients have suffered a brain injury and should be treated appropriately, said James C. Jackson, PsyD, a neuropsychiatrist at Vanderbilt University School of Medicine. “The old saying is that if it walks like a duck and talks like a duck, it’s a duck,” said Jackson.
He contends that treatments used for patients who have brain injuries have also been shown to be effective in treating long COVID–related brain fog symptoms. These may include speech, cognitive, and occupational therapy as well as meeting with a neuropsychiatrist for the treatment of related mental health concerns.
A New Path Forward
Treating long-COVID brain fog like a brain injury can help patients get back to some semblance of normalcy, researchers said. “What we’re seeing in terms of brain injury biomarkers and differences in brain scans correlates to real-life problems that these patients are dealing with on a daily basis,” said Jackson. These include problems at work and in life with multitasking, remembering details, meeting deadlines, synthesizing large amounts of information, and maintaining focus on the task at hand, he said.
There’s also a fear that even with treatment, the aging of the brain caused by the virus might have long-term repercussions and that this enduring injury may cause the early onset of dementia and Alzheimer’s disease in those who were already vulnerable to it. One study, from the National Institute of Neurological Disorders and Stroke (NINDS), found that in those infected with COVID-19 who already had dementia, the virus “rapidly accelerated structural and functional brain deterioration.”
“We already know the role that neuroinflammation plays in the brains of patients with Alzheimer’s disease,” said Thompson. “If long COVID is involved in prolonged inflammation of the brain, it goes a long way in explaining the mechanism underlying [the study’s reported] brain aging.”
Still More to Learn
In some ways, this study raises nearly as many questions as it does answers. While it provides concrete evidence around the damage the virus is doing to the brains of patients who contracted severe COVID-19, researchers don’t know about the impact on those who had less serious cases of the virus.
For Ziyad Al-Aly, MD, chief of research and development at the Veterans Affairs St. Louis Health Care System, the concern is that some long-COVID patients may be suffering from cognitive deficits that are more subtle but still impacting their daily lives, and that they’re not getting the help they need.
What’s more, said Al-Aly, it’s unclear whether the impacts of the brain damage are permanent or how to stop them from worsening. Researchers and clinicians need a better understanding of the mechanism that allows this virus to enter the brain and do structural damage. If it’s inflammation, will anti-inflammatory or antiviral medications work at preventing it? Will steroids help to offset the damage? “It’s critical we find some answers,” he said.
“SARS-CoV-2 isn’t going anywhere. It will continue to infect the population, so if this is indeed a virus that damages the brain in the long term or permanently, we need to figure out what can be done to stop it,” said Al-Aly.

Sarah Carter is a health and wellness expert residing in the UK. With a background in healthcare, she offers evidence-based advice on fitness, nutrition, and mental well-being, promoting healthier living for readers.