Researchers at Tel Aviv Sourasky Medical Center have successfully frozen an amputated limb in a rat, thawed it, and then retransplanted it back into the rat’s body with successful results.
A month later, the rat was able to walk normally. Although this breakthrough has so far only been demonstrated in rats, the researchers hope it could one day help limb injury patients regain lost limbs.
The research was led by Professor Eyal Gur, a specialist in facial nerve paralysis surgery and former head of the Department of Plastic Surgery at Tel Aviv Sourasky Medical Center, and Professor Amir Arav from the University of Miami’s School of Medicine and Chief Scientist of A.A. Cash Technology. They were joined by Dr. Nir Shani, former head of the Plastic Surgery Laboratory, Dr. Ina Solodeiev, who succeeded Dr. Shani, Dr. Sujin from China, and Dr. Or Friedman, a former resident in the department.
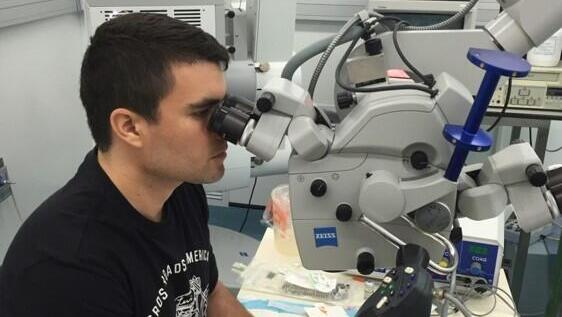
While the field of microsurgical reconstruction in plastic surgery has been around for decades, the technology required to achieve this breakthrough has only recently matured. “Fifteen years ago, I established a lab within the department to study reconstruction in plastic surgery and microsurgery—the ability to connect blood vessels and nerves less than a millimeter in diameter using specialized equipment,” said Prof. Gur.
During that time, Prof. Gur met Prof. Arav, who was working on preserving ovaries in women requiring pelvic intervention after chemotherapy or tumors. “The experiment succeeded, and we went our separate ways for many years. He continued advancing his research, and about a decade ago, we reconnected. He proposed that we try to freeze and then reattach an entire limb, aiming to do the same with human body parts—be it a hand, leg, cheek, or any other part.”
The rat a month later – able to walk normally
The freezing method that made this possible was developed by Prof. Arav in the early 1990s. The technique, known as vitrification, has also been used for freezing eggs and embryos in recent decades. “I developed this technique in 1991. It involves turning a liquid material into a solid state without forming ice crystals, making it physically solid but chemically liquid—similar to glass,” explained Prof. Arav.
Three years ago, the team made their first significant breakthrough when their experiment resulted in the limb remaining viable for several days post-transplant. “We published the experiment, but of course, it wasn’t enough,” said Prof. Arav. He described the process as complex: “You have to amputate the limb, freeze it at extremely low temperatures using liquid nitrogen, and then thaw and reattach it, reconnecting blood vessels and nerves. However, the technology wasn’t yet suitable for large tissues and organs, and that’s where progress stalled.”
Four years ago, they began applying this method to limbs, focusing on two key changes: cooling speed and preservation temperature. “We performed the process in a rat—amputating the leg, freezing it for several days, and then reattaching it, including reconnecting blood vessels, bones, and muscles. To our delight, after a month, we saw that the rat was using the leg just like its original limb. We had successfully preserved a leg through freezing and brought it back to life.”
 Prof. Amir Arav
Prof. Amir AravThis research was published last year but initially received little public attention. It eventually caught the eye of the Rosalind Franklin Society, which supports under-the-radar scientific work, and the study gained significant interest. The society even awarded it the Best Tissue Regeneration Research of 2023.
“This is a true breakthrough,” declared Prof. Arav. “Since the publication, we’ve expanded our work to tissues that are notoriously difficult, if not impossible, to freeze, such as fat tissue, ovarian tissue, or pancreatic tissue with the potential to produce insulin. We’ve successfully experimented with all these and plan to move forward to clinical trials in humans.”
Given the recent Iron Swords War and the high number of limb injuries in Israel, the researchers believe this development holds exceptional promise. “This research is highly relevant and poignant,” said Prof. Gur. “During the Iron Swords War, many lives were saved thanks to the extraordinary medical efforts by the IDF in the south, but there were also many limb injuries. The body was protected, the head was protected, but many soldiers lost legs—some below the knee, some both legs.”
“If we had devices in the field capable of freezing those parts and transporting them with the soldier to the medical center, where he would undergo intensive care, the soldier could be in a coma for a month, but his limbs would be preserved. Once stabilized, we could thaw the limbs and use them to restore the limb or repair other damaged areas. This offers an extraordinary, innovative hope for the field of reconstruction.”
Prof. Gur added, “Today, we often have to graft tissues from other parts of the body because we haven’t been able to save the amputated limb. While plastic surgery has its limitations, we’ve already broken through some barriers: One of the things plastic surgery can do is transplant organs from foreign donors, like faces and limbs. This requires anti-rejection drugs, which shorten life and cause severe complications. There’s nothing better than transplanting a patient’s own tissue, so if we can reach a point where we can reattach frozen organs from the same person, we’ll have achieved a phenomenal breakthrough.”
“The next step is to advance the experiment to larger animals and eventually to humans,” Prof. Arav concluded. “I believe that with the method we’ve developed, we’ll be able to transplant hands or legs below the knee. Our technology is patented, and we’re preparing for a fundraising round to bring this to fruition.”

Sarah Carter is a health and wellness expert residing in the UK. With a background in healthcare, she offers evidence-based advice on fitness, nutrition, and mental well-being, promoting healthier living for readers.