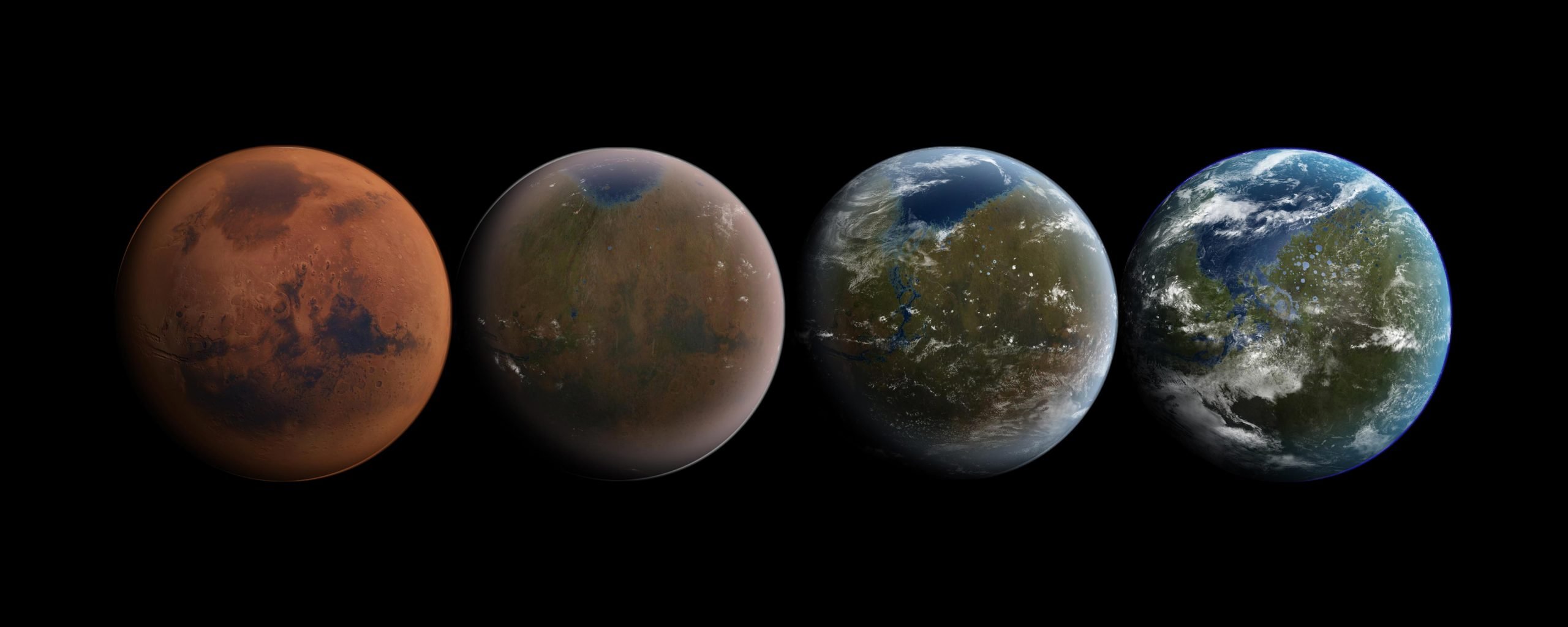
As she poses jubilantly for a photograph at Everest Base Camp, Corinne Turnbull, 51, looks the picture of fitness.
Conquering the world’s highest mountain is a challenge few of us would contemplate. But in Corinne’s case, that smile of triumph was especially hard-won – as just over a decade earlier, shortly before her 40th birthday, she was diagnosed with the bone-thinning disease osteoporosis.
I recently wrote in this newspaper about my own shock at discovering I had the condition, which up to that point I had associated with shuffling old ladies. My diagnosis came after I fractured my shoulder while training for a half marathon – I tripped on a tree root and fell awkwardly. A week or so later the hospital offered me a bone-density scan, known as a DEXA, which is made available to anyone over 50 who has had what’s called a ‘fragility fracture’. This is defined as a broken bone from a fall at a standing height or less. The team at the Fracture Liaison Service at St Thomas’ Hospital in South London gave me the upsetting news that I had full-blown osteoporosis.
It came as a major shock. I’m in my 50s, at the peak of my career and I regularly run the four miles from my home to the office, so it felt as though I had been hurled from robust, capable maturity to being labelled frail and feeble.
But I soon found out I am far from alone. My article generated a huge response, with readers writing in to share similar stories.
Tens of thousands of British women in mid-life or even younger are facing osteoporosis and juggling the agony of broken bones with the usual challenges of jobs, kids and relationships.
It is thought that half of the women aged over 50 around the world will break or fracture a bone because of osteoporosis.
The condition affects men, too, but eight out of ten patients are women as a result of hormonal changes that occur during the menopause altering bone density. Too often they find it hard to obtain scans, diagnoses and treatments. They may endure years of frustration and fractures before receiving the support they need.
Osteoporosis can take a heavy psychological toll, causing loss of confidence and self-esteem. Spinal fractures may cause unwelcome physical changes, such as a loss of height, a curved spine or a more protuberant tummy.
The sooner women are diagnosed and offered treatment, the more chance they have of living well with the incurable, but manageable, disease.
That’s why The Mail on Sunday has launched our War On Osteoporosis, a vital campaign that aims to tackle the situation with three simple demands.
Firstly, make Fracture Liaison Services available in every NHS Trust so all bone-break victims over 50 can be assessed for osteoporosis. I was fortunate to be referred to one, but these are not available everywhere in England and Wales, often meaning that cases go undiagnosed until they’re severe.
Secondly, a risk assessment for bone weakness should be included in the free health checks offered by the NHS to people aged 40 to 74. This would be supremely simple, adapting an existing questionnaire that is produced by the Royal Osteoporosis Society.
And finally, screening for risk of a hip fracture – which can be catastrophic – should be introduced from age 70. This would involve offering women a DEXA scan at this time in their lives.
Due to lack of provisions in her area, Corinne – who works in the financial services industry and lives in Hove, East Sussex – waited six months to get a diagnosis after a fall in the street left her reeling in excruciating back pain. She says: ‘The GP was not thinking about osteoporosis at all. When I did have a scan, it found I had seven vertebral fractures and a broken hip. If there had been greater awareness, perhaps they might have caught me earlier.’
This was despite Corinne having suffered from an eating disorder as a younger woman – a known risk factor for developing osteoporosis.
‘I had a very bright career, I had achieved a lot and travelled the world,’ she adds. ‘Other women my age were raising young families, but I had this condition associated with 80- and 90-year-olds.’
Since being diagnosed, Corinne has lost about three inches in height – the condition causes the bones of the spine to crumble and collapse – a fact which, she says, made her feel ‘quite ashamed for a long time’.
‘I spent a lot of time carrying the shame around by myself, like a really heavy sack of bricks,’ she says. ‘Now I feel the more it is talked about, the better. Osteoporosis is with you for life, so you have to manage it, not let it manage you. Everest was a version of that journey – I felt I had conquered the world. I know now I can do anything.’
Corinne’s bones have strengthened and she has not had another fracture since. She is taking hormone replacement therapy (HRT) containing oestrogen, which helps combat bone-loss. There is an array of drugs that can help manage osteoporosis, too, but these are often not offered to younger patients and have not been tested on premenopausal women.
Valerie Farr, 45, lives in Warrington, Cheshire, with her husband, Mike, and her two children Douglas, seven, and Chloe, four. She was diagnosed with pregnancy-associated osteoporosis in 2018. This is a rare form thought to be caused by high calcium demands of the foetus and in producing breast milk. But it took clinicians nearly two years after Douglas’s birth to find out what was wrong.
‘People had been telling me I had problems with my core muscles and with postnatal depression,’ she says. ‘When I found out I had fractured two vertebrae, it was bittersweet. It was confirmation I hadn’t been making up my pain, but on the other hand I had osteoporosis at the age of 40.’
Valerie wants access to a daily injection called teriparatide. It stimulates the cells that build bone and has been shown to reduce the risk of broken bones – particularly spinal fractures. In the UK, though, it is licensed for use only in women who have been through the menopause, though doctors offer it to younger women in rare cases.
The view in the medical profession is that most premenopausal women with osteoporosis don’t need drug treatments until they are older. The reasoning is that, in most cases, their absolute risk of a fracture will remain low until they move into later life.
Valerie adds: ‘I have had to jump through so many hoops. It is really galling to know there is a drug that could help me but told I won’t get it. This is destroying lives. But if osteoporosis was dealt with earlier, with access to medication and screening at the right time, there would be far fewer fractures.’
Lois Ainger, 44, also says she had to ‘fight’ for drug treatment, in her case with risedronate – a medication taken in tablet form which slows the break-down of bone.
The civil servant, who lives in Eastleigh, near Southampton, had fractured her hand in 2018 and was eventually found to have osteopenia – a weakening of the bones that is not as severe as osteoporosis – when she was in her late 20s.
She says: ‘I was in so much pain. That fracture was a big wake-up call. It has an impact on your mental wellbeing – the fear when I get older that I might not be able to pick up a bag of shopping.’
Lois would like to see trials on drug treatments for younger patients. ‘There is no research on the drugs on premenopausal women,’ she explains. ‘Why do we not have the same access to drugs? Why is there no research?’
Emily Cox was still in her late 20s when she was diagnosed with low bone density in a scan after suffering two fractures within a year.
The 44-year-old mother-of-two, who lives in Northampton with her daughters and her husband, Pete, found out she had the gut condition coeliac disease in her mid 20s – a well-known risk factor for weaker bones. Along with severe digestive discomfort, the condition also disrupts the absorption of nutrients, which then leads to osteoporosis.
Emily, who was diagnosed in 2022, says she ‘had to push’ for a DEXA scan despite being a high-risk case.’
She is now taking weekly tablets and is very active with her job as a pilates teacher, as well as running half marathons in her spare time.
‘I want to educate everyone, especially women, about the importance of keeping on with exercise when you have osteoporosis,’ Emily adds.
Elisa Sgubin, 48, from London, was diagnosed with severe osteoporosis when she was 40. She juggles the effects of the condition along with her career as a manager at a cruise company.
Finding the time to exercise – which helps boost bone-health – is a big challenge.
‘I know I need to exercise but I work long hours,’ Elisa explains, who describes her osteoporosis as ‘severe’. ‘Despite being careful, every year I have broken something. I have fractured my spine and broken my shoulder several times.’
Elisa is taking HRT and hopes in the future to be prescribed romosozumab – a drug approved by the NHS in 2022. The treatment slows the cells that break down bone matter and also stimulates those that build new ones. It is licensed for postmenopausal women, too.
Elisa concludes: ‘The thought of ending up in a wheelchair, of not being independent, of not being able to get on a flight – it’s always with me. Although it is not easy, I stay positive no matter what. I hope there will be new treatments.
‘Osteoporosis is not researched enough. We have to raise our voices, in the UK and all around the world. People need to hear us, everywhere.’

Sarah Carter is a health and wellness expert residing in the UK. With a background in healthcare, she offers evidence-based advice on fitness, nutrition, and mental well-being, promoting healthier living for readers.